Our anatomy is who we are physically, how we grow and how we age, the outcome of our genes and our diet, an evolving display of our health and our diseases. For millennia we have sought understanding of our structure by dissection of cadavers, which became foundational training for medical education. In much of the world such a vital learning resource is unavailable for logistical, economic, legal and /or religious reasons; where human dissection has been a rite of academic passage, such programs are now reducing or eliminating cadaver anatomy to make room in curricula for the sciences of future healthcare such as genomics. Yet the global population and numbers of elderly are surging, many living longer while suffering chronic diseases, creating unprecedented demand for more well-trained physicians and every other category of healthcare provider. Another major trend worldwide has been the increased reliance on diagnostic imaging technologies – CT, MRI, ultrasound, etc. – instead of the “laying on of hands” for physical diagnosis leading to therapeutic decision-making of the past, another fundamental change for future caregivers.
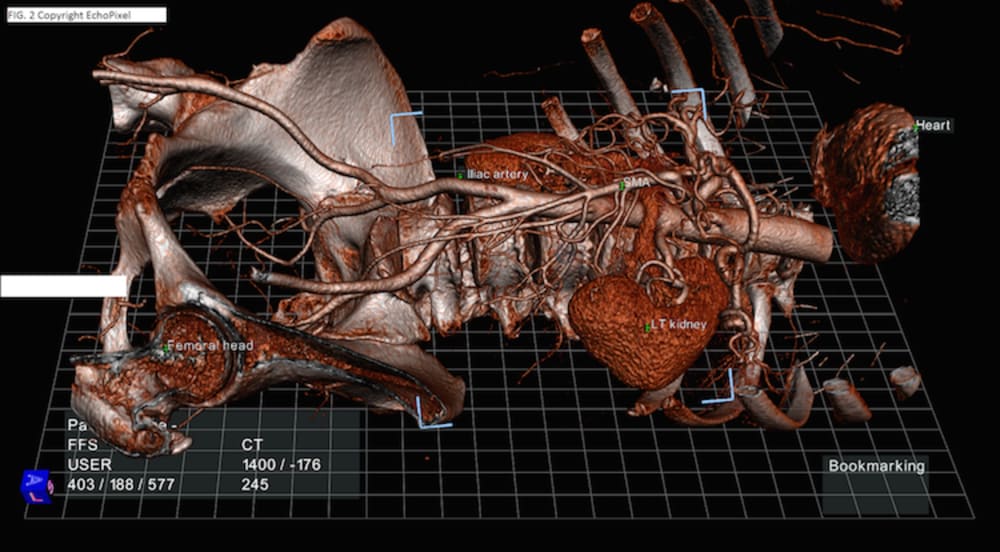
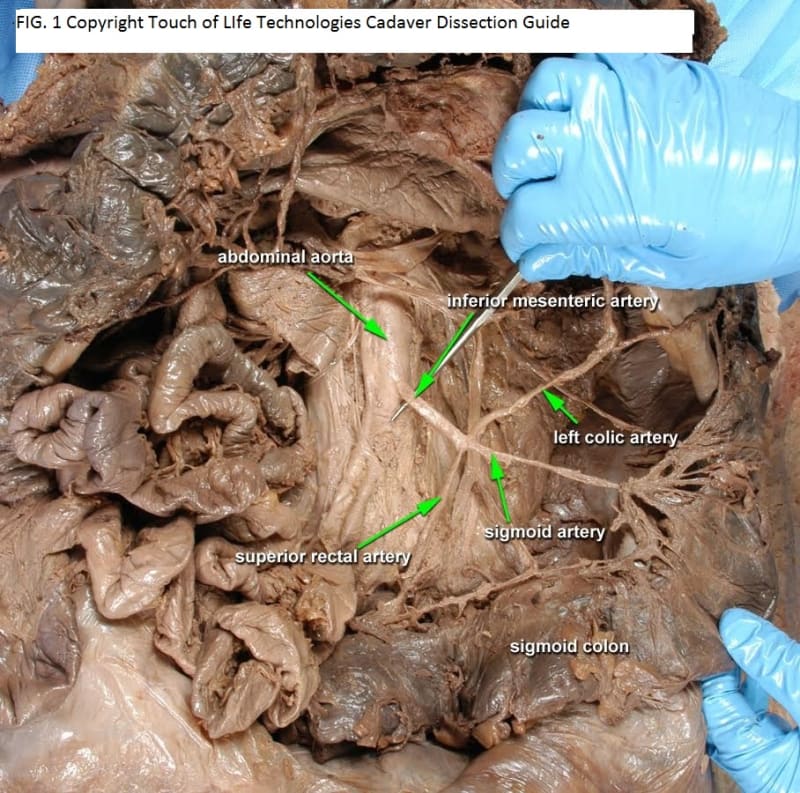
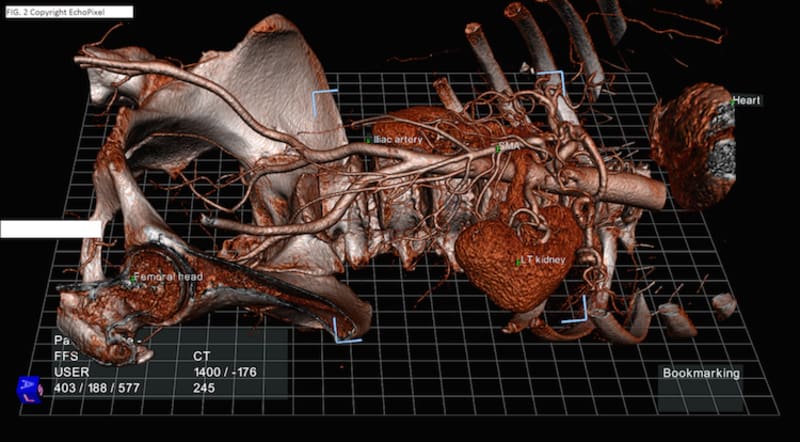
Technology offers an innovative solution to this imposing anatomic training challenge. Drawing on prior experience as a NASA Johnson Space Center contractor, we can create interactive, anatomically accurate virtual people, simulating both dissectable cadavers and treatable patients. The key to their interactivity is haptics, the experience of tactile interaction with virtual objects which display physical and textural properties. Using 3D scanning we can create any body shape, size, gender, and populate it internally with complete anatomic datasets such as the Visible Human and academic collections (Fig. 1). To that can be added extensive libraries of pathologic presentations and their impacts on human structure. A key innovation is the incorporation of DICOM imagery comparable to the anatomy of all body regions (Fig. 2) to reinforce the ability to master learning anatomy in 3D, and to interpret the DICOM data for patient care decisions. With haptics the virtual patient can be examined by palpation with hands, feeling masses, pulses, etc., and with a stethoscope, learning to hear and understand heart, lung and bowel sounds.
This project offers numerous advantages: Unlike physical cadavers which must be maintained in secure locations with limited access, our virtual cadavers and patients will be available 24/7/365 on diverse computing devices; unlike the large costs of maintaining a cadaver lab’s facilities, bodies, records and personnel, and similar great expenses associated with mannequin patient simulator purchase, maintenance, programming, etc., our virtual people will be available at reasonable subscription costs; current and future patient care in many countries is dictated by the economics of insurance and care facility costs, not appropriate patient management, leading to a dire shortage of clinical learning opportunities for students and residents to follow the course of a patient from diagnosis, through therapy to outcomes, while our virtual patients can manifest all possible consequences of a patient’s clinical course, from complete recovery to death, safely replicating the realities of healthcare. DAVID is prepared to help educate YOUR future doctor.
-
Awards
-
 2015 Top 100 Entries
2015 Top 100 Entries
Like this entry?
-
About the Entrant
- Name:Robert Rice
- Type of entry:teamTeam members:Robert W. Rice, Ph.D.
Richard W. Rieck, M.D., Ph.D.
Stuart C. Gardner
Jeffrey L. Creasy, M.D. - Patent status:none