Problem: The subclavian vein is accessed in about 2 million central venous access procedures performed annually in the US. This could be for hemodynamic monitoring in critically ill patients, delivering chemotherapy, parenteral nutrition, and pacemaker lead placement. Unfortunately, 88,000 of these procedures will result in a painful and costly pneumothorax, or a collapsed lung, because the operator has inadvertently punctured the lung. Typically guided by ultrasound or fluoroscopic imaging, subclavian venous access requires physicians to navigate through a 3D space using a thin long needle while looking at a 2D projection. There is a need to better guide physicians in subclavian access procedures to reduce the risk of inadvertent puncture to the lung.
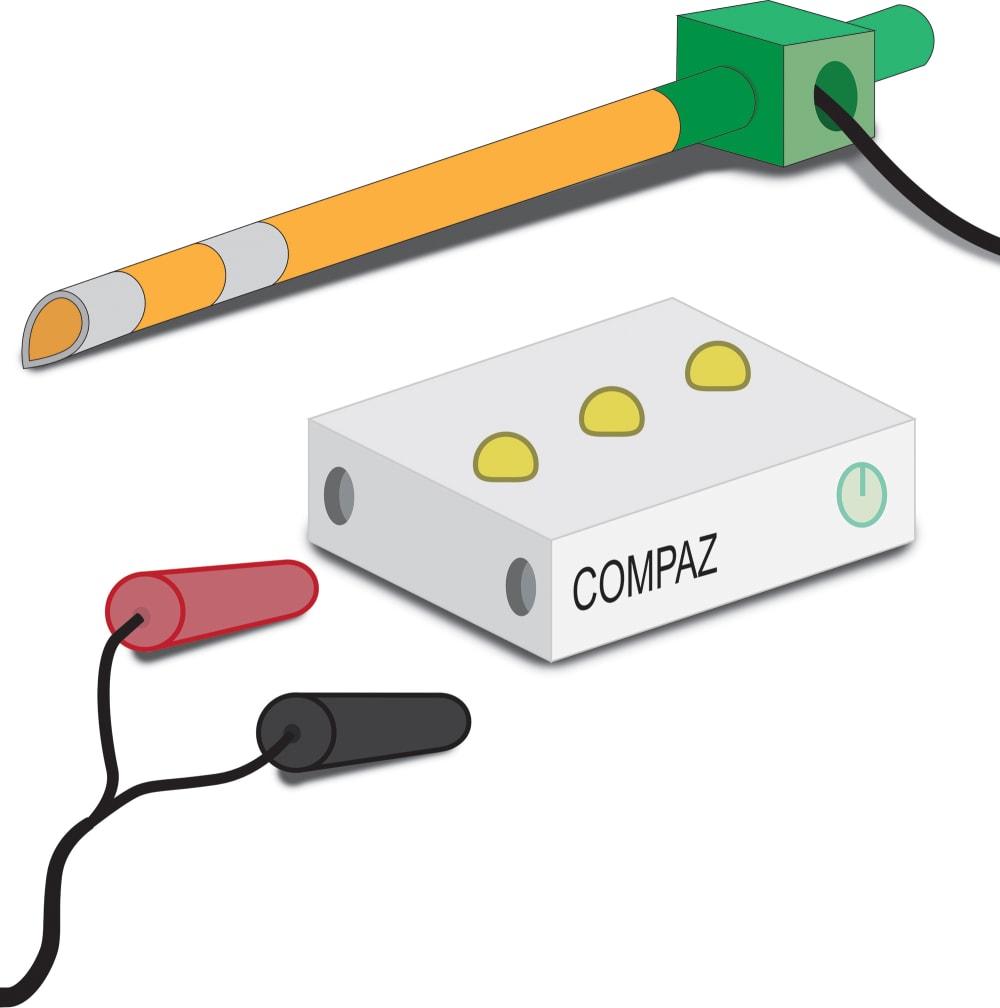
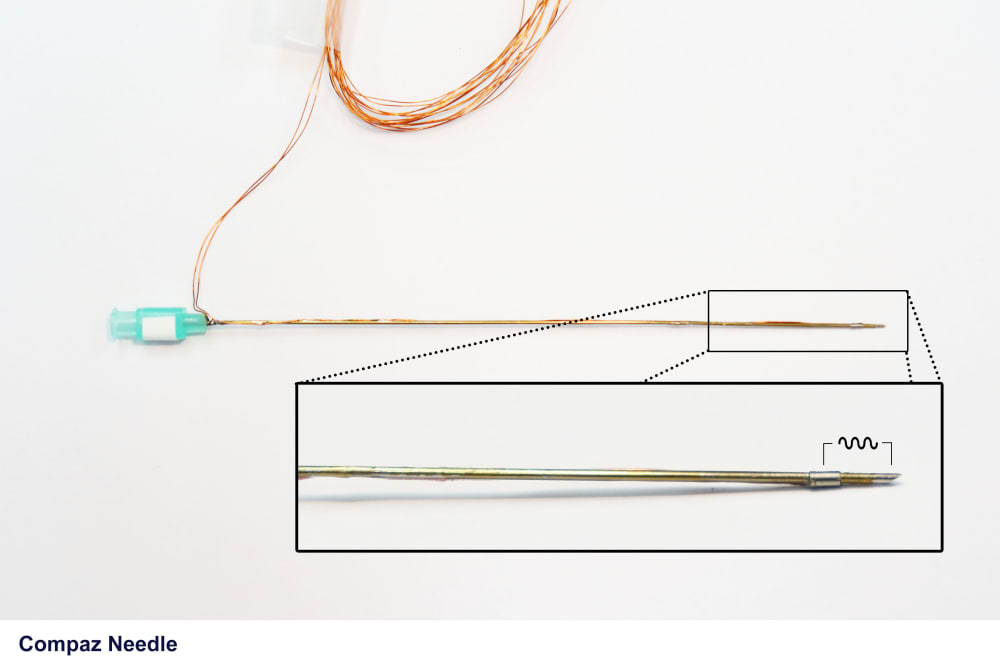
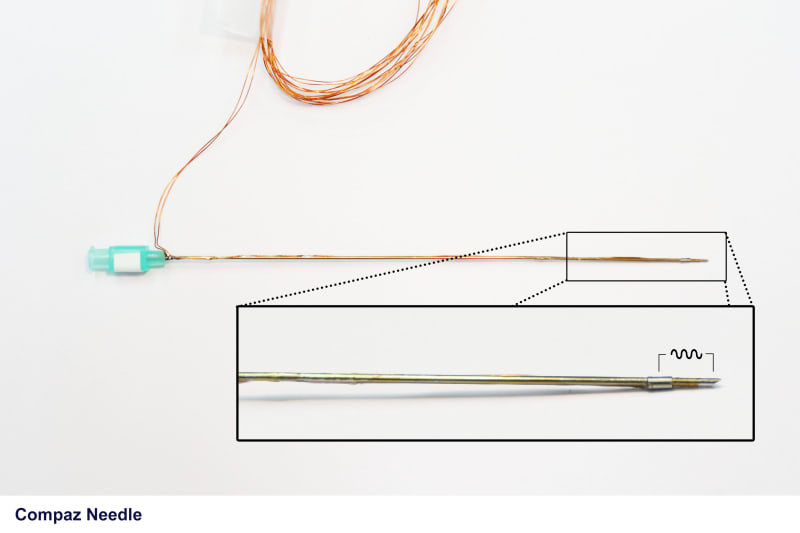
Innovation: The Compaz Needle system, developed by inventors at the Texas Heart Institute and Baylor College of Medicine, is comprised of a functionalized micropuncture needle that can be connected to a portable impedance analyzer that monitors real-time impedance that will supplement the existing access technology to prevent pneumothorax. Micropuncture needles have been attributed to a significantly reduced complication risk in comparison to their large bore counterparts. Electrical bioimpedance is measured at the distal tip of the needle, providing specific and spatially localized impedance feedback. Because tissues in the body have unique impedance values, the feedback from the needle can be used to distinguish the tissue surrounding the needle tip. Importantly, since the lung comprises primarily of air, we have shown that the Compaz Needle can clearly distinguish lung from surrounding tissues based on the impedance values. In the studies we have conducted impedance of lung could be differentiated from surrounding tissue with a sensitivity of 98% and specificity of 90% (AUC = 0.99). By indicating that the tip has just entered a lung space, the operator is notified by the Compaz Needle system and can retract and redirect the needle away from the lung. This will prevent a larger catheter or any such device from entering the lung and creating a pneumothorax. Not only can the needle help to avoid the costly complication of a pneumothorax, but it can help ascertain venous access based on the impedance measurement. We have demonstrated that the needle can differentiate the blood in a vessel from any other tissue with a sensitivity of 85% and specificity of 87% (AUC=0.87).
Manufacturability: The needle system and the impedance analyzer can be manufactured using cost-effective methods that is typically used for manufacturing needles and circuit boards.
Marketability: A pneumothorax can cost the hospital on average an extra $17,000, a cost that can be avoided using this technology. It can also increase hospital stay by 5-6 days. Additionally, surveys of physicians and clinical operators indicate concern for the potential for a pneumothorax 100% of the time this needle access procedure is performed. The Compaz Needle system can better guide physicians during venous access procedures. Our revenue model, where the needle is sold separate from the analyzer, has the potential to break even with the exhibited demand within a few years of first sale.
Like this entry?
-
About the Entrant
- Name:Mathews John
- Type of entry:teamTeam members:Mehdi Razavi, Texas Heart Institute
Allison Post, Texas Heart Institute - Software used for this entry:LTSpice
- Patent status:pending